
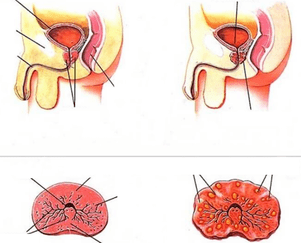
Chronic prostatitis is an inflammatory disease characterized by lesions of the prostate gland and severe urodynamic disorders. One of the causes of chronic inflammation of the prostate is improper or untimely treatment in the acute stage, when the desquamation and proliferation of the glandular epithelium is reversible and is successfully corrected by medication within 2-3 weeks.
Treatment of chronic prostatitis includes massive antibiotic therapy aimed at eradication of the infectious pathogen, a set of measures to increase the body's immunoresistance, physiotherapeutic methods, thermotherapy. Psychocorrection can also be included in the therapy regimen, since neurasthenic and neurosis-like conditions are often observed in men with long-term and recurrent prostatitis.
Why does inflammation become chronic?
Knowing the causes of chronic inflammation of the prostate is necessary to prevent exacerbations and improve the quality of life of patients. There are a large number of factors that can affect the functional state of the glandular (glandular) tissue of the prostate gland and cause its inflammation, which is based on desquamation and proliferation of epithelial cells.
The main cause of chronic prostatitis in men is the extensive contamination of the mucous membranes of the genitourinary system with pathogenic microorganisms. In the overwhelming majority of cases (more than 80%) of infectious prostatitis, gram-negative and gram-positive bacteria become the causative agent of infection: enterobacteria (in particular, Escherichia coli), gonococci, staphylococci. Less often, the infectious and inflammatory process proceeds against the background of infection with viruses, fungi and protozoa, but such forms of prostatitis are quite successfully treated during the acute period and rarely give relapses, subject to correct and timely therapy.
It should also be borne in mind that for the development of chronic aseptic prostatitis, a single acute infection of the urinary tract is sufficient, therefore, personal hygiene, the use of condoms during intercourse and timely treatment of diseases of the urinary tract are of great importance in the prevention of this disease in men. Medicine knows cases of hematogenous (through the systemic circulation) infection of the prostate in chronic sinusitis, tonsillitis and other diseases that contribute to the active growth of pathogenic flora, therefore, sanitation of foci of chronic infection is an important stage in complex treatment for prolonged or protracted inflammation of the prostate.
Negative factors that can cause exacerbation of prostatitis (including non-infectious course) are:
- urinary tract injuries and surgery on the organs of the genitourinary system;
- regular or severe hypothermia of the pelvic organs (swimming in open reservoirs during periods when the water is not warm enough or the weather is cool outside, work in refrigerators and freezers, etc. );
- hypodynamia caused by sedentary work and insufficient physical activity of a man (a sedentary lifestyle is one of the main factors in the development of chronic cognitive prostatitis);
- bad habits, in which the absorption of the most important macro- and microelements that determine the chemical composition and rheological properties of prostate secretion (zinc, chromium, selenium, manganese) is slowed down or impaired;
- disorders in the intimate sphere (frequent masturbation, irregular sexual relations, long periods of abstinence, frequent arousal, not ending with intercourse);
- overweight;
- eating disorder (increased consumption of spicy, too salty, smoked and fatty foods).
Pay attention! Urologists note that the leading pathogenetic factor in the development of chronic inflammation of the prostate is posterior urethritis. It was also noted that inflammatory changes in the prostate in men appear during the first months after a gonorrheal infection.
Treatment of chronic prostatitis with drugs
Treatment of chronic prostatitis with medication is aimed only at suppressing acute symptoms during an exacerbation and destroying the infection, but drugs cannot be used as the only means (the effectiveness of such treatment will not exceed 36%, according to Dr. Pechersky).
A complete drug treatment regimen for protracted or recurrent prostate inflammation that is used today as a standard in uncomplicated disease is presented in the table below.
Table. Preparations for the complex treatment of chronic prostatitis.
| Pharmacological group | Purpose |
|---|---|
| Antibiotics from the group of macrolides, semi-synthetic penicillins and third-generation cephalosporins with a broad spectrum of antibacterial activity. | Eradication (destruction) of pathogenic bacteria - causative agents of infectious prostatitis, urethritis, cystitis and other urinary infections. |
| Antimicrobial and antiprotozoal agents. | Treatment of infections caused by pathogenic microbes and protozoa. |
| Non-steroidal anti-inflammatory drugs (preferably in the form of rectal suppositories). | Reduction of inflammation in the tissues of the prostate, relief of pain in the perineum, intergluteal space, sacrum and groin. |
| Antiseptics in the form of rectal suppositories. | Rehabilitation of rectal mucous membranes and prevention of its infection with prolonged prostatitis. |
| Alpha blockers. | Normalization of urination, restoration of daily urine output. |
| Microcirculation correctors. | Elimination of congestion in the vessels of the small pelvis, restoration of normal blood and lymph flow. |
| Correctors of urodynamics (agents affecting the metabolism in the tissues of the prostate). | Improvement of metabolic and metabolic processes in the tissues of the prostate gland and its nutrition. |
| Potency regulators. | Complex treatment of erectile dysfunction, improving the chemical composition, viscosity and fluidity of seminal fluid, increasing sperm activity (the use of drugs of this group is indicated for patients whose prostatitis is complicated by autoimmune infertility). |

The duration of antibiotic treatment is at least 4-6 weeks. In no case should you take medicines with an antibacterial effect without a doctor's prescription, since the leading factor in the selection of therapy is the results of microscopic examination of prostate secretions and fluids spontaneously released as a result of prostate massage. Some antibiotics, for example, penicillins (a combination of amoxicillin with clavulanic acid) are reserve drugs, and their incorrect use can lead not only to the absence of a clinically significant effect and the progression of the pathology, but also to the development of superinfection.
Important! In some cases, men with chronic prostatitis need psychocorrection, especially if the pain syndrome is combined with behavioral changes, increased anxiety, irritability, and neurasthenia. Antidepressants with selective serotonin reuptake inhibition are used to suppress these symptoms.
Physiotherapy
Heat therapy is the main method of treating chronic prostatitis outside periods of exacerbation (after regression of acute symptoms). Heat therapy refers to the methods of physiotherapy and is a dosed effect of heat on the affected area. The benefits of thermal procedures are in the normalization of blood circulation, relief of inflammatory processes, reduction of chronic pelvic pain, which is one of the main clinical manifestations of chronic prostatitis, which reduces the quality of life for men. Heat also improves the penetration of medicinal substances into the prostate tissue, so in some cases physiotherapy is used to increase the effectiveness of drug therapy (for example, electrophoresis with antibiotics). For men with a high risk of thrombosis, warming is prescribed for prevention, since heat has a moderate resorbing effect.
There are a large number of methods of thermal effects on the body, and the choice of a specific treatment method should be carried out by a doctor, taking into account the clinical picture, the form and stage of the disease, the age of the man and his individual tolerance. The following thermotherapy methods are most effective for prostatitis:

- thermal applications with minerals (ozokerite, paraffin, bischofite), salt or sand;
- electric heating pads;
- deep heating of high-strength tissues for direct action on blood vessels and nerve endings (diathermy);
- exposure to high-frequency alternating magnetic fields to eliminate pain, relieve inflammation and eliminate neurosis-like manifestations (inductothermy);
- ultrasound therapy (promotes resorption of abscesses and healing of formed scars);
- electrophoresis with the introduction of electrodes into the rectum;
- impact on the prostate tissue with high frequency impulse currents (darsonvalization).
In some physiotherapy rooms, chronic inflammation of the prostate is treated with hot mud applications ("mud pants"). Such procedures have a positive effect not only on the circulation of blood and lymph, but also on the production of prostate secretion, as well as tissue nutrition of the inflamed organ. In some cases, mud is injected directly into the rectum in the form of tampons, since with this method of administration it is possible to quickly achieve a therapeutic effect and a positive response to the therapy.
Other treatments
The scheme of complex treatment, in addition to drug and heat therapy, is supplemented by various procedures that the doctor prescribes, taking into account the peculiarities of the pathology in each case.
Prostate massage
This is one of the main methods of treatment of chronic inflammation of the prostate gland, which is advisable to use in almost 90% of cases (in the absence of contraindications). Massage is a finger effect on the prostate in order to stimulate the outflow of secretory fluid. The duration of the procedure is usually about 1-2 minutes. The criterion for a sufficient effect is the complete emptying of the prostatic glands, which the patient feels as relief (which he should inform the doctor about).
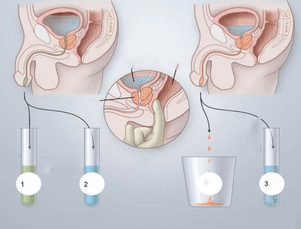
The benefits of massage are determined by the therapeutic effect that can be achieved after undergoing a course of treatment (8-12 procedures). With an uncomplicated course, these are:
- normalization of muscle tone;
- improvement of blood circulation in the vessels of the prostate (due to this, the transport of medicinal substances into the tissues of the affected organ is accelerated and the effectiveness of therapy is increased);
- restoration of secretory patency;
- normalization of the outflow of blood and lymph from the prostate gland (especially significant in cognitive prostatitis).
The procedure is contraindicated during the acute period due to the high risk of spreading the infection to the surrounding tissues and organs (hematogenous infection), with other infectious diseases of the genitourinary system, the presence of cysts or stones in the prostate. Massage of the prostate is not prescribed for patients who have been diagnosed with tuberculous organ damage, adenoma or other neoplastic diseases (including cancerous lesions of the prostate gland). In the presence of diseases of the rectum (hemorrhoids, anal fissure, proctitis, paraproctitis), the massage can cause complications and provoke a relapse of the underlying disease.
Important! Studies show that almost 42% of men refuse prostate massage due to the increased psychological discomfort associated with the peculiarities of this procedure. The physician's work with such patients should include detailed information on the consequences of refusing treatment and possible complications, in particular, infertility and persistent sexual dysfunction. In some cases, it may be advisable to prescribe light sedatives a few days before starting treatment.
Hot enemas
Hot enemas are home treatments for chronic prostatitis, but urologists recognize their effectiveness and recommend them for faster and more effective treatment of prostatitis. The water temperature for these enemas should be around 42 ° C. Before the procedure, it is necessary to cleanse the intestines with a regular enema or laxatives. The volume of one enema is from 150 to 300 ml. It is recommended to empty the bowel 30-50 minutes after the administration of the solution.

Recipes for chronic prostate inflammation are listed below.
- Dissolve 10 drops of iodine and about 20 ml of chlorhexidine in 200 ml of water. Apply at bedtime for 15 days.
- A decoction of chamomile, St. John's wort or calendula should be introduced into the rectum (about 250 ml), and then keep it for 1 hour. The procedure is repeated once a day for 2 weeks.
- Sea buckthorn oil (40-50 ml) is heated to 40 ° C and introduced into the rectum for 20-30 minutes. The course of treatment is 10-15 days. The procedure is best done before bedtime.
- In case of severe pain syndrome, which significantly limits the patient's mobility and worsens his quality of life, microclysters with novocaine can be used. Dissolve 2 ampoules of a 2% solution of novocaine in 180 ml of a steep decoction of chamomile. Hold for at least 50 minutes. Repeat daily for 1 week.
Anti-inflammatory drugs, antiseptics, antibiotics can also be used from medicines for microclysters. The use of these drugs is permissible with the permission of a doctor strictly in the indicated dosage.
Treatment of chronic prostatitis: step by step instructions
The use of various methods of treatment is not enough to completely get rid of chronic prostatitis. If a man does not monitor his diet and does not change his lifestyle, exacerbations will occur regularly, leading to irreversible changes in the structure and functional activity of the prostatic glands and persistent dysuric and sexual disorders. For the effectiveness of treatment and the duration of remission to be higher, you should adhere to the recommendations set out in the instructions below for patients with chronic prostatitis.

- Step 1. If a man is diagnosed with chronic prostatitis, he should start by correcting his diet. It is necessary to exclude foods with a large amount of fat, salt and spices from the menu. Fats increase blood cholesterol levels, and salt promotes fluid retention and edema in the prostate tissue. Spices (like various chemical additives) irritate the mucous membranes of the urinary tract, provoking an exacerbation of existing symptoms.
- Step 2. It is also necessary to completely eliminate alcoholic beverages, as they slow down the absorption of nutrients, disrupt the circulation of blood and lymph, and negatively affect the metabolism in the prostate. If a man suffers from tobacco addiction, measures should be taken to get rid of this habit (toxic substances in tobacco smoke violate the viscosity and fluidity of prostate secretions and change its chemical composition).
- Step 3. Overweight men should consult an endocrinologist and nutritionist for a comprehensive diagnosis and correction of body weight, taking into account the identified deviations. Obesity is the most important factor in the development of chronic prostatitis, and an important stage in complex therapy is weight loss in patients with high BMI.
- Step 4. To eliminate stagnant phenomena associated with hypodynamic disorder, it is necessary to provide an adequate level of physical activity, corresponding to age and physical fitness. Swimming, physiotherapy exercises, stretching exercises, walking are useful for prostatitis.
- Step 5. For the normal functioning of the prostate it is necessary to monitor the quality of sexual life. It is advisable to have a permanent sexual partner, to avoid episodes of sexual arousal if there is no possibility of further intercourse, and to be regularly checked for genital infections, which can also provoke an exacerbation of chronic prostatitis.
Men with recurrent prostatitis need to monitor emotional stress, avoid stressful situations, as well as prolonged exposure to cold or drafts.
Chronic prostatitis is a disease that is difficult to treat, especially if the patient does not follow the prescription of the attending physician and does not take a responsible approach to the issues of nutrition and regimen. Inflammation of the prostate is dangerous with serious complications, so you need to approach the problem comprehensively. Men with this diagnosis should understand that pills alone are not enough to completely restore all functions of the prostate gland, so you should not abandon the methods of basic therapy for chronic prostatitis suggested by your doctor, even if they cause primary psychological or physical discomfort.






























